a creative non-fiction story formulated over a decade ago and only recently completed (it still needs some polish)
MEMORANDUM THRU Commander, SHAPE Medical Clinic, SHAPE, Belgium
TO Director, SHAPE Liaison Office, Ambrose Pare Hospital, Mons, Belgium
SUBJECT: Patient Comments/Suggestions
1. After breaking the bone in my upper left arm, I stayed four days in the Ambrose Pare Hospital. I was admitted the morning of 16 March thru the emergency room. I was out of the operating room (after receiving a metal bar with eight screws) and awake by mid-afternoon. I checked myself out, against my surgeon's request, on 19 March.
2. I was asked by SHAPE Liaison Personnel and by Dr (CPT) Shiltie to prepare a comment form, documenting my dissatisfaction. I list here, not only the reasons I refused to remain in Ambrose Pare, but positive aspects of my experience. My hope is this After Action Report is used as a basis for changing the changeable, informing future patients, and commending the commendable.
3. POC is the undersigned.
VEACH GLINES
CW2, USA
AFTER ACTION REPORT - AMBROSE PARE
1. Situation - Contact with Patient Liaison: After a quick examination at the Base Medical Clinic, I was told my broken arm may require surgery and that Ambrose had been called. "They know you are enroute." A nurse said, as she handed me a form to provide to the Ambrose Pare admissions clerk as I walking out to my friend's vehicle.
Upon entering the Ambrose Pare's Emergency Entrance, I approached the admissions clerk who spoke only French. I gave her the form and filled out another, in English. I asked for SHAPE Liaison (SL) assistance. I was given words of affirmation and directed down a hall to an unknown location. Unable to understand where I was being told to walk I stayed put, waiting for SL. A doctor coming to work stopped when he realized my confusion and guided me to X-Ray.
Result: I never met any SL personnel in the Emergency Room, after X-Ray, while waiting for surgery, or in the recovery room. After I was in the hospital more than 7 hours, already in a room on the first floor, I met a SL member who asked if I had any questions. By that time all my questions were moot.
Solution: When the Admissions Clerk greets a foreigner with as poor a command of the French language as mine; it should be automatic that he or she calls the cell-phone or pager of SL and punches a code indicating they have an ER admission who is (as I was) disoriented, in pain, scared and unsure of what directions he is being given. The ER should be given highest priority by all SL personnel. If tied up with something of higher priority (e.g. translation of a conversation between a patient and his surgeon, on the table, seconds before going under the knife) then meeting the patient as soon as physically possible is acceptable. If this isn't SHAPE Liaison Standard Operating Procedure (SOP), it should be.
Comment: I realize the SL has a limited staff and they can only be in one place at a time. They also have only two hands and I know they are very busy. I met every member of the staff during their long (0800-2400) workday on the four days I was in the hospital. I greatly appreciated all their assistance and would not have stayed as long as I did if it weren't for them.
2. Situation - No Communication: Permission to operate on my arm was never asked for or given. Because I am familiar with the US's over-protective system it was quite a shock to be wheeled into surgery and have my body being prepared for operation when I had yet to be told why I was going to need surgery or authorize it by signing a waiver of any type.
Result: I met my surgeon two minutes before I was placed under anesthesia. He spoke enough English to answer my questions and calm me. If he had arrived any later I would have had the surgery with no idea what was happening other than the guess given to me by the SHAPE Medical Clinic personnel hours earlier.
Solution: Add to the SL SOP, the additional priority of having a SL member present prior to surgery.
Comment: This is not a criticism as much as a reminder. Anyone who lives at SHAPE knows as a general rule the local Belgians do not know much English. Just because they are working in a hospital doesn't change anything.
3. Situation - Drug Reaction: My known allergies were Penicillin and Erythromycin. I must now add to that an unnamed morphine-based painkiller. I was given an intravenous drip of painkiller every four hours or so following my surgery. There was no noticeable reaction to this drug all through the day and through the night and next day (other than I fell asleep and felt little pain).
Very early (approx. 0100) on the day after my surgery, I felt very uncomfortable and unable to sleep; I was given a big shot of painkiller. My allergic reaction consisted of extreme spasms to the muscles covering my abdomen. Those muscles affected my ability to breathe (diaphragm), my ability to keep my back and leg muscles straight, and my contortions caused more pain than the drug was able to mask, causing me to involuntarily move the un-protected broken arm.
Result: Unable to relax my muscles voluntarily I called the nurse. She interpreted my actions and hand/arm signals to mean I was in need of a bedpan. I indicated she misunderstood and I didn't need a bedpan. I tried to tell her I was having stomach spasms because of the shot. She brought me a laxative and had me take it, indicating it should take effect in 12 hours or so. I gave up and asked for the SL. The nurse informed me they would come see me after 0800 when they got to work. My drug addled (the drug was still doing it's job, just doing some other stuff too) brain quit trying and spent over two hours of sweating and pain before either the side effect wore off or the painkiller caused me to pass out, or both.
Solution: A booklet or laminated, reusable, pamphlet needs to be prepared that contains the English (and other languages that are needed) and French phrases which may need to be used on a "can not wait" basis. This should contain phrases like, "I am experiencing a bad reaction to a drug causing my (blank) to (blank)." Then include lists: stomach, head, arm; convulse, vomit.
Other phrases, for example: "Please contact my wife and allow me to talk with her." may be useful for a person unable to hold a phone. "Contact my surgeon, there is a emergency or problem with my operation," may be a sentence needed when there is no time to pantomime.
Comment: This seems like a common statement here at SHAPE: every time is the first time for every thing. But, it's all fun and games until someone pokes an eye out (or breaks a bone). I felt like I was the first non-French speaking person to reside in this hospital and have problems. An SL person told me that I wasn't the first person to have difficulties, just the first person to become so agitated and unpleased with the hospital to leave against my doctor's orders.
4. Situation - No Pain Medication (The pain problem continues): After informing the SL of my reaction to the pain shot, I was not given any more pain medication, ever. I requested the SL members to tell the nurses I needed more, just different, pain medication (as I had done the day before when the nurses were being typically stringent with their pain killers). The SL said all I had to do was 'tell the nurses' (not one nurse knew the word "pain", they must have thought my arm was baked bread). The SL also told them for me.
And I cornered the orderly who removed the drain tube from my arm. He knew he caused me much discomfort while removing the tube and he was as knowledgeable in English as I am in French. He told me I had to wait for the '12 hours to expire' then pointed at the medication drip.
Result: I never got any more pain medication (except aspirin and later an alka-seltzer-type dissolving medicine; neither medications touched my pain). From the time I woke from the "bad shot" on day three until I checked myself out the evening of day four, I received no pain medication (except my own aspirin).
Even then, I had to wait until sick-call Monday morning to get a prescription for painkillers from SHAPE. I was unable to sleep Saturday night more than 30 minutes at a time, total of about three hours. Not all caused by pain: a hospital is a busy place, I had a roommate, nurses have checks and no one whispers. Sunday night was home and quiet, but the discomfort caused me to sleep very little.
Solution: If this wasn't just miscommunication or an error in the way the Ambrose Pare's nursing staff normally conducts patient care, then either some direction needs to be given to the nursing staff or SHAPE should reevaluate utilizing this hospital as an authorized care providing facility. Doors to patient rooms should be left in the closed position unless it is visiting hours, allowing the normal hustle and bustle of the nurses, orderlies, and cleaning crews to be minimized.
Comment: My pain was minor compared to someone with burns or extensive trauma. In my opinion, miscommunication and error were not the reasons I was left without painkillers for over 30 hours. I think the nurses need instruction on nursing. As a layman, I would know enough to check on my patients and discover they seem to always be awake when I'm in the room. Then determine why.
Note: I should add here that I stopped requesting pain medication after about 12 hours. I'd asked five or six different people and gotten nothing that worked. I was afraid they would grow tired of my asking (if all six were going to one central person who was refusing each time, as I envisioned) and administer another "bad shot" possibly after SL departed for the evening again.
This paranoia was caused by many different things, some of which may have been drug or pain induced. Mostly, however, it was because I understood a small amount of the nurse's words (and all of their body language and facial expressions) to know one thing: they despised dealing with me.
5. Situation - Orderlies: Morning of day two and I was beginning my first sponge bath by two orderlies who were apparently college girls. Both were visibly embarrassed to be required to bathe a man. I was unable to leave the bed. My broken left arm had a drain tube running from a six-inch incision into a vacuum bottle under my bed; my right arm had an equally large bandage holding the IV needle into which ran two drips.
The orderlies had already begun and informed me the only areas of my body they were going to wash were my legs, arms, armpits, chest and face. No they were not going to wash my hair, back, genital area, or shave me. Before they could wet a cloth, my wife arrived. They asked if she would like to assist. I pictured her doing the parts they refused to do and holding up legs while they scrubbed, things like that. She agreed to help. They left and never returned.
Result: My wife spent over an hour washing and shaving me. Because my wife's complete body wash and shave was so much better than the orderlies' wipe-and-go program. I asked her to return the next day at the same time. She did. And the nurses related she could also return to wash me on day three, which she also did.
Solution: The orderlies are in need of guidance on how to clean a body. If that means having a male orderly wash all male persons and vice versa, so be it. The fact that a patient is using bedpans and bed urinals should be more reason to wash his genitals than any other. The hair and back of a person become so dirty from body oils and sweat that to not clean them leaves one's personal hygiene completely lacking. Again, I recommend a close examination of the patient care abilities of Ambrose Pare. If they are not able to make changes then I recommend placing the hospital "off limits" to all military and their dependents.
Comment: It is possible that other patients who have previously used Ambrose Pare have either not concerned themselves with orderlies abilities, they may have been able to wash themselves (which would preclude noticing this lack of hygiene) or they may not have been witness (as I have with an elderly family member) to the correct "sponge bath technique". Regardless of why, I can't be the only person who would have left with the same dirt on my buttocks that I came in with, if it weren't for my spouse. Prior to this, I was aware how most French-Belgians had a strong body odor and how, in general, they were unclean. I did not know that it extended to hospital hygiene.
6. Situation - Visiting Hours: After my wife finished cleaning me Friday morning, a nurse came and asked if my wife was done. When informed she was almost done, the nurse left. 15 minutes later a different nurse came and told us that visiting hours were from 1500-1930. This was the first either of us had been told of these hours.
Result: My wife left and returned at 1500. Between her (not normally allowed) morning bath and 1500 I had no one to talk with, nothing to do (TV is solely French, I couldn't hold a book or phone longer than two minutes) except concentrate on my discomfort and fail all attempts to go to sleep.
Note: The Solution and Comment portions of this paragraph are combined with those of the following paragraph, because these two problems have similar solutions.
7. Situation - Private Room: After waking in the recovery room, I vaguely remember answering questions from the bottom of a blurry well. One of those questions was (all being asked by my surgeon; I doubt if this is normal either) what kind of room did I want? My answer was a private one...except...also...within whatever the US Military was going to pay for (proving I was merely groggy, not delirious).
Result: I was put in a room with four beds and two roommates. A SL person asked me on Friday afternoon if I, "still wanted to be moved to the private room" and then she told me why it would not be her recommendation.
The SL person said the cost of a private room was about $150 US dollars each day above the cost of the 4-person room which was what is covered by the military; also the hospital and operation room/doctor fees could be increased anywhere from 100% to 200% (not determined prior to receipt of the bill) and all increases would be my responsibility. She used figures in the thousands of US dollars. I opted to remain in the room I was in.
Solution(s): Either military CHAMPUS coverage or Ambrose Pare Administration needs to change the allowable/charged room rates and the "undetermined increase of fees" to permit SHAPE personnel to have private rooms without any additional cost to the service member, because the visiting hours for persons in private rooms are 0800-2000.
Also needed is a "Welcome Letter" from the SL Office, to all arriving patients. It would benefit the most if it were automatically handed out by the admissions clerk (both in ER and at the front doors). This letter would outline all routine functions of the hospital including, but not limited to, visiting hours, room options, clearly defined costs for benefits not covered by the military, services provided and supplies needed. Note: Robes, towels, washcloths or slippers are not available or provided. No water or beverages are provided except during meals.
Note: The combination of alcohol and pain medication is not a concern. I was offered a beer with lunch on Friday. I declined because I was wary of mixing alcohol and medications.
Comment: If my wife were permitted to remain in a multiple-room during private-room visiting hours, the other members of the room could object. However, I witnessed first-hand how this rule was easily bent when it benefited the nurses by permitting them to do less work (not bathe me).
8. Situation - Incompetence: In the early morning hours of day three I observed my drip tube was no longer dripping (when you can't sleep, you look at anything to pass the time). I notified the night nurse. She tried checking the bag; it was operating all right. She attempted to force fluid into my arm by squeezing the small rubber boot attaching the tube to the "T connector" taped to my arm. This failed attempt caused fluid to move in and suck back out of my arm. She repeated this painful attempt two or three more times. The nurse then disconnected a tube from the "T connector", sucked fluid through it using a small syringe, determined the connector was working and then she attempted to force the fluid into my arm by squeezing the syringe. I came up off the bed with more pain in that arm than the other. She quit forcing the fluid and left glaring at me like it was my fault.
Result: She removed the IV. The swelling and bruising caused by the forcing of the fluid into a collapsed vein was very evident. She placed a large compress on the wound, covering the entire wound with some of the most fowl smelling black-tar ointment I have ever had the misfortune to have to breathe.
Solution: Again, if this is the normal practice of the Belgian Nursing community, then instruction and specifically Ambrose Pare's standards should be examined. If this was just a coincidence, and they normally don't cause undue pain to their patients, then that specific nurse should be evaluated as to competence.
Comment: Based on the fact the tube temporarily stopped prior to the bag being empty and other nurses and one orderly also squeezed the rubber boot causing me pain, I believe this is common practice. She just took it further.
9. Situation - Lax Nursing Staff: After removing my "ace bandage" wrap and all gauze bandages in the afternoon of day two, the orderly responsible for removing my drain tube left the room. He returned with a nurse. She examined the exposed arm and then asked me if my wife was returning at 1500. I told her yes and she asked if my wife was still going to wash me. I was not sure what she was asking (since my morning bath was already done for that day) but said yes. She told the orderly my wife would clean my arm later and left the room.
Result: I learned by stumbling through both his English and my French that he had asked the nurse to clean the dried blood, adhesive, and medicinal stains off my arm. The orderly was merely responsible for removal of the tube and then redressing the sutured area and re-wrapping the arm; the nurse was supposed to clean it. He then asked me if I wanted the arm to be cleaned under the bandage or if the bandage should be left off until my wife cleaned it. I asked him to clean it and re-apply the wrap.
Solution: Examine the Ambrose Pare nursing staff and their supervisors. Obviously, none are required to perform to any standard of patient care.
Comment: Again, the nursing staff is culpable of shirking their responsibility. The orderly, however, was quite efficient.
10. Situation - Cleanliness: On day three, in the late morning, I was able to leave the bed and go to the sink in the bathroom to bathe. Allowing my wife to clean me without having to use a pail of water. Some water got on the floor. She used a paper tissue to clean up the water. The tissue was so dirty after just wiping up a small amount of water that I would hate to see how much dirt would come up if a scrub brush and strong soap were used.
Result: I observed how the ladies, responsible for cleaning a room, performed their duties. They used a "Belgian broom" type instrument (sponge with a dry lint adhesive towel under it) to push-sweep the central areas of the room. Not under beds, not in the bathroom, not anywhere the half-meter-wide tool wouldn't fit. Then they used a buffer with an automatic wax applicator to raise a shine in the central areas of the room. Dusting was done on horizontal surfaces (table tops, headboards, etc) No one did anything in the bathroom besides run a brush around in the bowl and wipe the sink. I did observe some wetness on the floor of the bathroom, but it was only enough wetness to cause the dirt to become wet, not to pick up any of it.
Solution: A change is required. This change needs to come from within the hospital. A standard must be enforced and inspections made to insure they are maintained. Give a date to have the hospital "up to code" if they cannot pass the inspection of a chosen military official. Deny Ambrose Pare the SHAPE community's business. (I just hope St Joseph's hospital isn't a carbon copy).
Comment: A hospital is where cleanliness is expected. Allowing our military members and their families to utilize facilities that are below any acceptable cleanliness standards is unforgivable.
11. Situation - Urine Bottles: I was only able to urinate in a urine bottle until my IV was removed on the morning of day three. I quickly noticed that when I used the bottle, and a nurse or orderly dumped it into the toilet, they never rinsed out the bottle.
Let me re-enforce this statement: Not sometimes, not usually, not almost never. NEVER. Not one of the dozens of times that my bottle was taken by one of the Ambrose Pare nursing or orderly staff during my three days of constant IV fluids did the sink in my bathroom get turned on and my urine bottle rinsed after dumping the urine in the toilet.
Result: To use the bottle, I had to open the wet cap of the urine bottle and place the wet mouth of the urine bottle at my groin. Then after filling the bottle, I would place the bottle on my bed-table and wipe my hands and genital area on a towel or on the bed sheet.
Solution: This may be the easiest to fix. Ambrose Pare can make the general SOP change: All urinals are rinsed just like bedpans; I doubt that bedpans are returned coated with feces (although I don't know, I was unable to use a bedpan).
Comment: Common sense (forget hygiene and medical training) tells you to rinse out the urine bottle. My thirteen year old (not known for hygiene or common sense) would probably do it instinctually!
12. Situation - Bed Pans: I was constipated. It was possibly the food (a topic I will not critique here, if there is a gourmet hospital in this world no one I've known has been there). It may have been the drugs combined with lying horizontal for days. Regardless, I couldn't use a bedpan. No nurse commented that I needed to try (except the nurse who mistakenly thought I was asking for one) and, as far as I know, no nurse ever knew that I had gone a minimum of four days without a bowel movement. That added lower abdomen pain was the capper on my good humor.
Result: I requested the SL ask the nurse if I could use my own laxative from home. Initially, the SL person gave her opinion ("I don't think they want you to bring in your own medication") But I persisted and she agreed to ask the nurses. They permitted it. I used it. It also didn't work so I had to resort to the most uncomfortable means of forcing a bowel movement.
Solution: Is this enough "Nursing Failure" comments? The solution is simple. Insure the Ambrose Pare Nurses are not just ladies off the street with pink and white dresses that know how to read a thermometer, blood pressure gauge, and say 'no' to pain medication.
Comment: In the past, nurses I've interacted with the few times I've been hospitalized, were concerned with how much I was "passing my wastes". They also were strict about when and if I get out of bed for fear of dizziness and falling. I got out of bed on day two so the orderly could change my bed linen. Less than 24 hours after surgery and I was dragging the drain tube and bottle and IV's over to a chair without any assistance.
13. Situation - Bed Linens: My wife washed me on day two and since she was not very familiar with the technique, she got water on the sheets and pillowcases. I told her it was no big deal, I saw a stack of clean sheets sitting in a chair and watched through the curtain as one of my roommate's bed was changed, so I knew I'd get clean/dry sheets. But, when I was in the chair, the orderly did not change the bottom sheet (stretching the length of the bed). The only sheets that were changed were the top sheet and a "protection" sheet that was across the middle of the bed under my buttocks. They also didn't plan on changing any pillowcases (one of mine was very wet from hair washing) so he had to go get a clean one, which took ten minutes.
Result: My bottom sheet stayed wet and soiled. It was never changed the entire time I was in that bed.
Solution: Change the hospital's procedures. All sheets are changed every day and more often as hygiene dictates.
Comment: Is this enough "lack of hygiene" criticisms? I was only in one room of one ward for four days; I can't be but just scratching the surface. We need an in-depth investigation with the health and well being of our military members in mind. The focus needs to be on our choice of health care providers and their standards. If they can't bring theirs up, are we expected to lower ours? At what expense?
14. Situation - Duration of Stay: On day three I asked the SL to contact my surgeon and ask him to visit me. When asked why, I told her I wanted to leave the hospital. I saw no reason to remain. I was actually more tense, less comfortable and the hospital, in my mind, was possibly more of a danger to me in terms of possible germs and diseases as well as errant nurses and incompetent orderlies (I left this last comment off, as I had done the entire duration of my stay. It's been my experience that one doesn't stir the pot when one is part of the stew). All I told her was now that my tubes were removed I could conduct all future business with my surgeon on an outpatient basis.
Result: My surgeon told me he wanted me to remain 48 more hours. His reasons were vague, but centered around, "After surgery a body needs to be watched, the skin and nerves, blah, blah."
Follow-on Situation: Almost immediately after my surgeon departed the SL person came, reiterated to me what the Surgeon had just told me and added I was being moved to a different room. When asked why, she replied because I was supposed to be on the second floor. She didn't know why I was put on the first floor. I had been there for four days, but now it was time to move me.
Result: I was moved from a room with one roommate who I had no difficulties with in any way (the second roommate moved my second day) to a room with three roommates. At the time of moving, each of the roommates had 2-4 guests in the room (one guest per roommate is about all a full 4-man room can handle without bothering a neighbor; two, if one stands...this should be a note of guidance in my proposed 'welcome letter').
At this floor, the SL person took it upon herself to ask my 'new' nurses if they were aware my wife had been coming in at 0800-0900 each morning and cleaning me and if that would be permitted on this floor. (I never asked her to ask them if that was permitted). I had learned from the nurse herself (on the first floor) that they were willing to 'look the other way' as long as my roommate didn't complain. I would have handled that situation similarly. She reported to me that the visiting hours would not be broken on this floor and my wife was not permitted to come the next morning.
Solution: I readdressed my surgeon and as tactfully as possible told him that under no circumstances would I stay in this hospital another night.
SUMMARY COMMENT: The SL members are always well intentioned but they allow their own opinions to enter into their conversations. I am fully aware of the difficulty of dealing objectively at all times; but professionalism demands it.
I learned from further conversations that a Belgian Citizen only pays a little over 40 US dollars extra for a private room. The reason is something about the national insurance covering all but that amount. SHAPE members don't have the insurance, so only the minimum is covered and the hospital sticks a large amount of hidden fees onto the bill (because they can).
Further, I recommend the 'Welcome letter' include detailed information on what to do for follow-up care. If you have an outpatient appointment (which can be made through the SL office) you must go to the front desk/cashier (any one of the three) and tell them your name, fill out another form, and receive a sheet of stickers. Then (and only with the stickers) can you get your x-rays and your surgeon's meetings as well as make additional appointments.
A map of the hospital denoting the ever-changing remodeling, and how to circumvent it, should also accompany this letter (words need to be in both French and English on the map so you can relate the map to the signs on the walls in the hospital).
Post Script:
Many months later I learned why if I was touched, even lightly, my arm hurt. I experienced (under the scar as well as near the elbow) excruciating pain, caused by a simple bump or nudge.
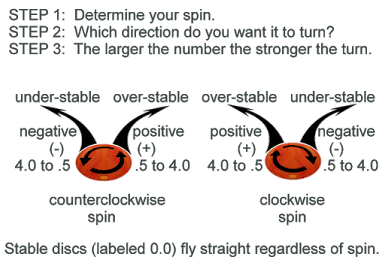
An x-ray revealed the eight screws were "counter-sink screws" but the metal bar did not have counter-sunk holes. Therefore, all eight screws had their sharp, angled, edges exposed inside my arm above the bar. Also, three of the screws went completely through the bone and projected their points under my bone near the elbow.
Bump my arm on top and the meat of my arm muscle rubs along the tops of the exposed screw heads. Hit the bottom of my arm on a table edge and the points of the screws try to puncture their way through my muscle and skin.
And I'd thought it was only the nursing staff that was slip-shoddy and incompetent.